Blog
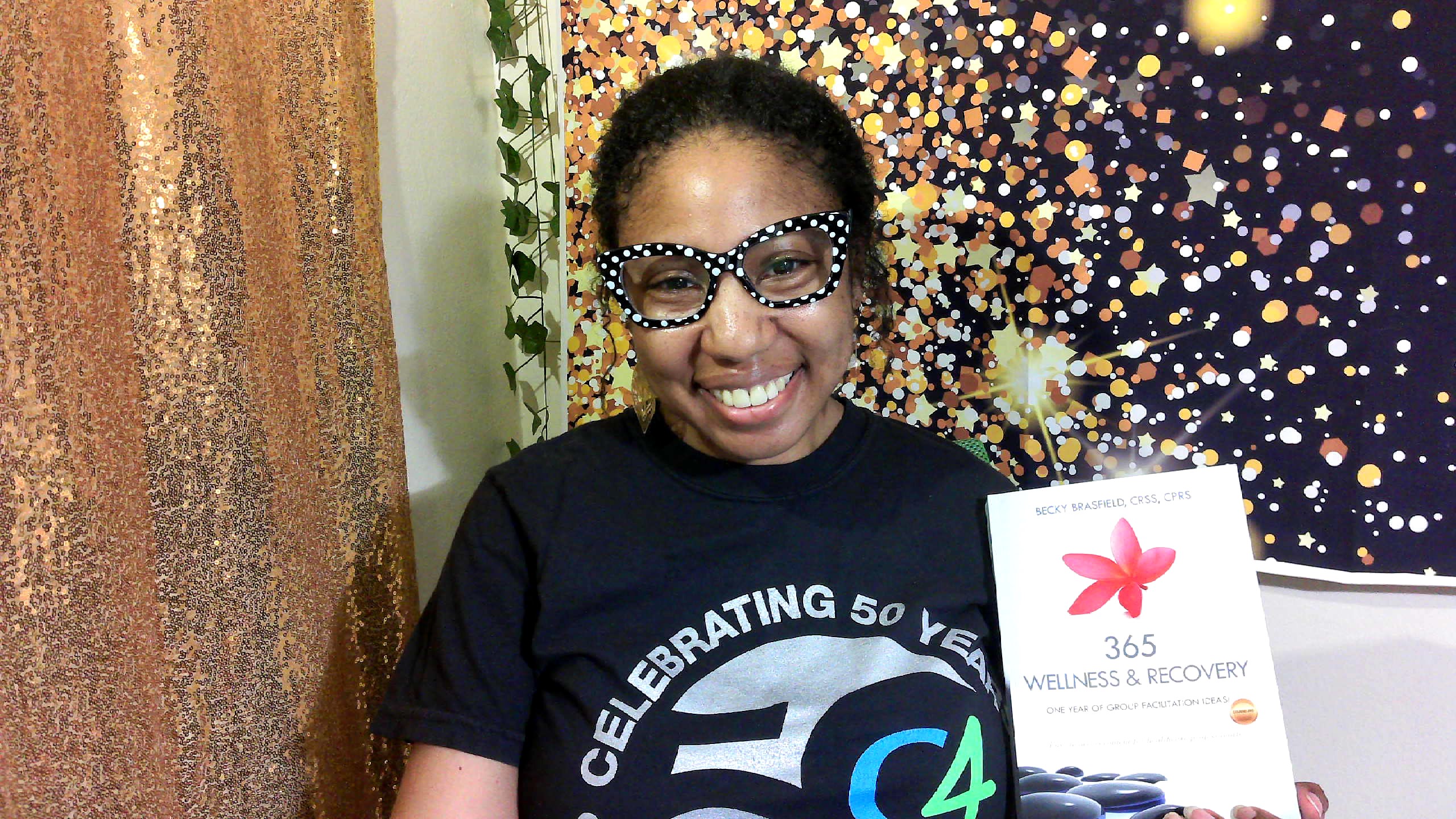
Employee Spotlight: Moniqueca Long
We sat down with Crisis Stabilization Clinician Moniqueca Long to talk about her work answering calls to the 988 Suicide & Crisis Lifeline. This interview has been edited for length and clarity.
Content Warning: This interview contains references to domestic violence, gun violence, and suicide.
Moniqueca Long: I’m Moniqueca. Besides my supervisor, I’m C4’s first 988 employee. I went to school at Roosevelt University. I studied sociology. During the pandemic I got a little more into social work. I didn’t complete a degree, but I kind of completed a lot of coursework in social work at that time, which got me into nonprofit work. Outside of C4, I’m a birth and postpartum doula.
C4: What about social work interested you?
ML: It kind of came with my conflict with sociology. I felt like with my sociology degree, I would never get to work with people. I would never be able to be impactful, I would never get a chance to have conversations, because a lot of that work is geared towards research and planning and things like that. So, I decided to make that pivot because I wanted to work with people. I’m very much a people person. I love talking, I run my mouth sometimes. I like to interact with people, and that was the first thing, but one of my points of pivot is that I really cared what happened to people outside of my time with them. I’ll be honest, I pursued several career paths to helping. I was at one point thinking about being a counselor, so pursuing a master’s in psychology, but I felt like it wasn’t encompassing enough to what people are experiencing. It kind of dealt with that cycle of perspective – not really thinking about all of the different factors that affect a person, or what I could do or what resources I could lend to support people.
C4: So you’re the first 988 clinician hired here. How long have you been at C4?
ML: Since August. I interviewed in July then came on right on August 8, actually. Not too far from a year, almost a year.
C4: Tell me about what a typical day looks like for you.
ML: I work remotely, so a typical day is number one just maximizing my self-care before I start work, because sometimes, the moment I clock in the phone is ringing and someone’s in crisis. I have to make sure I’ve taken care of myself, whether that’s eating a granola bar and milk or just kind of taking five minutes of silence, because the moment I’m on, I’m on. What’s interesting about my day is I never know who I’m going to talk to or what their story will be. Ideally, we talk to people all over the Chicagoland area – sometimes due to the area code they’re calling from, they could be in Louisiana or Las Vegas – but every time I talk to someone, I don’t know who I’m talking to. I don’t know what’s their story. It’s almost like watching a movie each time; you know the plot, but you have to listen to the details and the clues. Typically, I’m talking to people about something that happened today, something that’s been happening that’s brought them to a point where they feel worthless, or they feel like they’re contemplating taking their life.
C4: Were you familiar with the Lifeline or services like that prior to starting here?
ML: I’d heard of it. I never called; I never knew what to expect honestly, so not so much.
C4: Is the role matching your expectations of what it would be like?
ML: I think so. I think that what made me interested at the time was that I was working in a grant-funded program that was ending, but it was a violence prevention grant from ICJIA. And a lot of the youths there felt comfortable coming to me with all sorts of things. Oftentimes, I didn’t feel like I was really equipped to address some of those things. I wasn’t necessarily the right person, so my goal was just to listen to them and give them space, and that’s what made me confident in applying for this role. I was able to build relationships with people based on trust and just being a safe space for them.
C4: What makes this work important to C4 and the community?
ML: I think I tell everyone how important the work I do is. I joke, “I’m literally saving lives today, what are you doing?” But it’s so important because I talk to people that are probably around me in my neighborhood, that I would never connect with because we haven’t established that rapport. And what’s kind of jarring about it is that so many people have similar experiences that bring them to this place. They’re in situations where they feel really trapped, they don’t know what it is they want, or just no one’s ever taken the time to listen to them without that judgment. I think that what brings me to work every day is… I don’t want to call it “success,” but it feels successful to talk to someone about their life, and then at some point in the conversation they feel empowered. They’re recognizing their own strengths; they feel equipped to do this. And it’s not so much of what I’ve done, because we’ve only been talking for fifteen minutes. I’m not the expert in your life, you are. I’ve just asked you about your perspective and you’ve come up with this. I think that it’s so helpful because there are so many people who come to that point for different reasons. They’ve been on an escalating crisis for weeks, and then they hit this point and they’re reaching out for help because they can’t trust that anyone around them will help them without that judgment or without someone immediately wanting to call 911. It’s been very rewarding for me just to hear people feel empowered about their own lives and what they’ve already been doing and feeling like, “Okay, I can do this, and if I feel like I can’t do this, I’ll call back.”
C4: Could you tell us about an experience you had working with a client that helped you grow, and did it change the way you approach your work?
ML: Okay, so I have some issues with that question, because I’m going to be very transparent: I don’t think there’s a week I work that I don’t have a client that pushes me. I’m just thinking about the last few people I’ve talked to. There’s one caller who has severe mental illness who’s been living with this for years, so she knows coping strategies, she knows how to distract herself, but she’s still dealing with these very severe symptoms, so she calls very frequently. I was also talking to a mother whose son was a victim of gun violence, and he has siblings. And she’s really struggling with grief, but also with how to show up for her kids. I also think about a mother who had lost [custody of] her children, and she shared with me that she was thinking about killing herself because she’s using substances and she was also pregnant. She was in this very deep fear that this child would also be taken. So, when I think about all the people I talk to every time, there’s no way that I can pick one person, because everyone has caused me to learn.
I even thought about the time my supervisor, Hilda [Hernandez], coached me through getting someone out of an active domestic violence situation, even with the police there and the police leaving, and just showing me how that plays out in real life. I honestly cannot pick one, because in every situation I’ve learned. Even in that last situation with domestic violence, my supervisor really taught me so much. She has a background in volunteering in that type of work, so from that situation and what we talked about personally, that led me to teaching a group of doulas about domestic violence, because we are in the home and in close proximity to families and family violence. That gave me a really great opportunity to educate others about what this looks like, what to do if you see this, how can you support. I feel like I’m always having to grow, always having to research, always having to learn a new technique. Even with the Lifeline, they have so many resources and different sessions that you can drop in on, and through that session I came with one of my calls and they shared this really great technique to help with people with severe mental illness. So, I feel like I’m always being challenged to learn more, to learn different things, to learn from others with more experience in crisis work.
C4: Thank you for answering that so fully. Particularly given your role, having to adapt to that versus having a set caseload comes with a whole different set of challenges and keeps that growth going.
ML: And another thing is that it’s in real time. I don’t really have time to do a lot of research or reach out to anyone. You have to be very particular in what you say and deciding when to listen, when to try to engage more, deciding when you’re at the end of the road of support for this person. Maybe there’s a next level that needs to come in, but that would be MCR [Mobile Crisis Response]. We don’t automatically call law enforcement, because for a lot of people that would be disadvantageous. We want to maybe explain to people, “Well, I’m concerned about you. I think you could really benefit from doing the same thing that we’re doing but have someone come out and see you.” And not everyone agrees to that, understandably, but some people do take advantage. But yeah, crisis work is… real. It’s real.
C4: My last question is, what’s one thing you want people outside your sector to know about the work you do? And are there any common misconceptions or things you want to clear up?
ML: There’s two things. The number one thing that I want anyone to know is that you can help save a life. There are resources within the lifeline. There’s a really great resource called “Be The 1 To,” and I love sharing that resource because a lot of the people who are calling aren’t someone in crisis, but someone that’s worried about their loved one, or their friend, or their student, and they don’t know how to approach it or support, and they really want to support, but they think, “Oh, I’m not a psychiatrist, I’m not a counselor, I can’t do this.” And I tell them, “Well, I’m a clinician, and there are things you can do.” Number one is listening without judgement, hearing what they have to say. Asking them the question, “Are you thinking about killing yourself? Are you thinking about ending your life?”
You can also tell them to call 988 if you’re not comfortable, if that’s really outside your mental and emotional capacity. The other thing I want people to know is that when you call the Lifeline, when you’re talking to someone like me, my goal is never to take anything from you. I always want you to walk away with some type of self-awareness and that’s the interesting thing that thinking about ending your life does. It opens up the opportunity to learn what need you have right now that’s not being met. Oftentimes, there are multiple needs. And people usually think, “Oh it’s money, it’s this,” but sometimes it’s self-care. Essentially, I want you to know that I won’t call the police on you unless it’s completely necessary. That’s just something we don’t do. We don’t take away people’s rights, unless they tell us they’re on the Chicago River and they’re going to jump at 3 o’clock. And obviously then I have to do something. But if you’re telling me, “I’m having these thoughts about killing myself, I just don’t want to be here,” it’s never my goal to take away your rights or take anything from you. I just want to explore that and maybe bring you to a place of awareness of what it is that you want, what it is that you could do make things better, what would make things better? What is better, what would that look like to you? Oftentimes, people feel like when they call for help, they think I’m going to call 911. That’s the biggest thing. I don’t want to say we don’t [call 911], but it’s never our goal to involve law enforcement right away to arrest anyone or hospitalize when it’s not necessary. My goal is literally to deescalate. One really great activity I do with callers is I pick a category and I do the ABCs. So, I say, “You’re from Chicago, right?” and they usually tell me they are, and I say, “Okay, we’ll go through the streets of Chicago with the ABCs.” A, Ashland; B, Belmont; C, Chicago Avenue. And by the time we’re done – people really get stumped when we get to Q, no one thinks of Quincy – people’s brains are working so their body has a chance to reset from all the anxiety and stress they just experienced. And I tell them “Take that with you, that can help you when you’re feeling really, really overwhelmed and just reset. Like maybe I can’t do what my brain is telling me to do right now, but I can do this activity and then decide if I can return to whatever activity I was doing before it escalated.”
C4: Is there anything you wanted to add?
ML: I’m so excited that I get to talk about what I do. I’m glad I can talk about it to someone outside of my circle, like this is what I’m doing, this is how I help people.